
Pelvic Inflammation Disease or Pelvic Pneumonia is a condition that occurs when bacteria infect the muscles, tendons, tissues and organs in your pelvic region. Pelvic Inflammation Disease (PID) is a potentially dangerous infection that develops if certain sexually transmitted diseases or infections are not treated immediately. PID can also develop after a pregnancy because of high blood pressure and the effects of hormonal fluctuations.
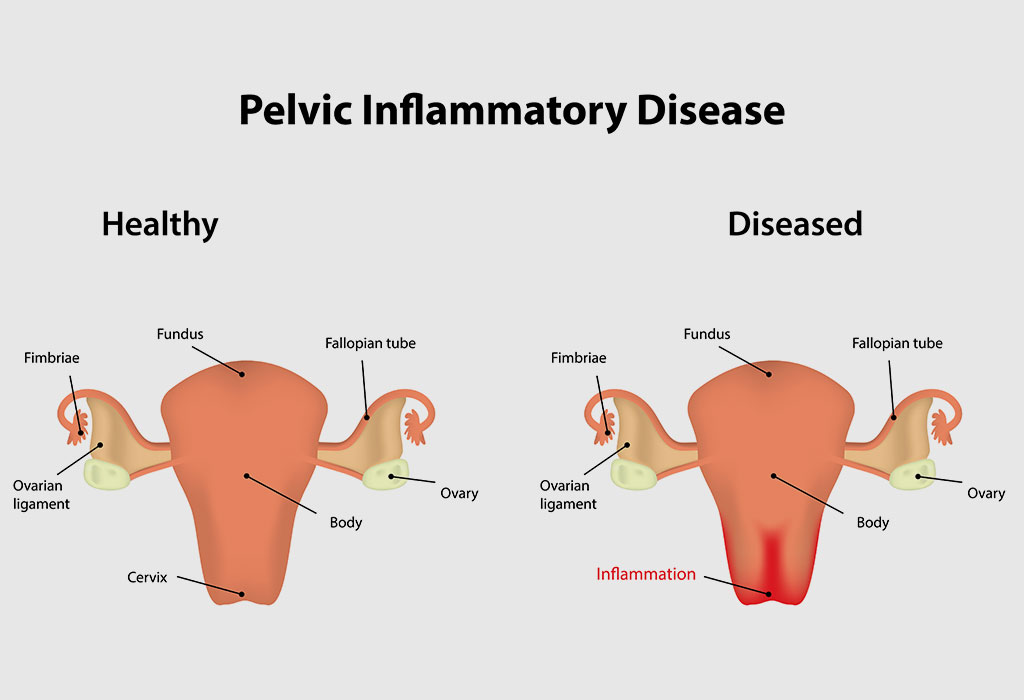
Pelvic inflammatory disease (PID) is an infection of the uterus, ovaries, fallopian tube, or both
The more you have PID, the more severe the symptoms tend to be. PID can lead to serious complications, including infertility if not treated promptly. Fortunately, PID is curable and can be treated with treatment options that can address the infection from the inside out.
If you suspect that you may have pelvic inflammatory disease, there are a number of possible causes. A variety of factors such as being pregnant, having diabetes, poor circulation, having multiple sexual partners, smoking, or use of antibiotics are potential culprits. If you are experiencing any of these symptoms, talk to your doctor about whether you may have PID.
Your doctor will perform a medical evaluation to confirm or rule out any possible infection. When a diagnosis has been made, you will be given a prescription for an anti-bacterial medication that can be taken by mouth, topically, or in the form of a cream or gel. If you choose to treat the condition using medications, you may also need to change your lifestyle.
Many medications may also be prescribed to help regulate your menstrual cycles and prevent complications during pregnancy. These treatments can also help prevent the spread of pelvic inflammatory disease to your baby. However, sometimes antibiotics can help control the overgrowth of bacteria. In some cases, your doctor may also recommend surgical options to remove the affected areas.
To relieve pain associated with pelvic inflammatory disease, you may need to use over-the-counter pain relievers. You should avoid taking aspirin or ibuprofen as these medicines can interfere with certain drugs, which could result in complications if taken together. Painkillers are also useful for dealing with pelvic inflammatory symptoms that occur after surgery.
Other medications that can help with the symptoms of pelvic inflammatory disease include herbal remedies. Herbal medicines that can be taken internally include black cohosh, witch hazel, clove oil and other products that can be applied directly to your abdomen or pelvic area.
Some medications are prescribed to reduce inflammation and ease discomfort while others are used for the purpose of pain relief. Corticosteroid creams can also be used to ease symptoms, but they should only be taken on a short term basis because they can actually worsen the symptoms of pelvic inflammatory disease. In most cases, surgery is needed to address the problem because it is not possible to eliminate the condition completely. In some cases, doctors may recommend a combination of medication along with a healthy lifestyle.
There may be times when your doctor will recommend surgery to treat your condition. If your doctor determines that you are at high risk for developing the disorder, he or she may prescribe you a hysterectomy. Hysterectomy is a major surgery that removes the uterus and the fallopian tubes.
Surgery is the only option that can be used to treat pelvic inflammatory disease in women who are not at high risk. If you have not yet reached menopause and are not pregnant, or if you are not ovulating, you should consider hysterectomy. surgery for pelvic inflammatory disease. If you already have had hysterectomy, there may be more serious underlying problems causing the disorder that needs treatment before resorting to a surgical procedure.
Your doctor may suggest a hysterectomy due to several conditions. One of these conditions is tumors that grow on the uterus. Other conditions that may warrant surgery are infections, pelvic inflammatory disease, cancer, or endometriosis. Sometimes, the uterus and fallopian tubes may be removed to make way for a better treatment plan.
Surgery is a serious procedure and you should expect to pay for the treatment out of pocket. Your health care provider will explain to you all the possible risks and benefits associated with the surgery, including the possibility of infection after the surgery.